Blog
MEDICAL DEVICE AI BUILT-IN VS MEDICAL CLOUD AI VS MEDICAL DEVICE HYBRID: A COMPREHENSIVE ANALYSIS OF ADVANTAGES AND DISADVANTAGES
Executive Summary
The healthcare industry is experiencing a transformative shift with the integration of artificial intelligence (AI) into medical devices and diagnostic systems. This comprehensive analysis examines three primary approaches to medical AI implementation: built-in device AI, cloud-based AI systems, and hybrid architectures that combine edge and cloud computing capabilities.
Built-in medical device AI offers real-time processing, enhanced data privacy, and reduced latency through on-device computation. These systems excel in point-of-care applications where immediate results are critical, such as the FDA-approved IDx-DR diabetic retinopathy screening system. However, they face limitations in computational power, update capabilities, and scalability.
Cloud-based medical AI systems provide superior computational resources, seamless updates, and enhanced collaboration capabilities. Platforms like Google’s Medical Imaging Suite and Arterys demonstrate the potential for complex algorithmic processing and multi-institutional data sharing. Nevertheless, these systems encounter challenges related to data security, network dependency, and regulatory compliance under HIPAA guidelines.
Hybrid medical AI architectures emerge as a promising solution, combining the immediacy of edge processing with the computational power of cloud systems. This approach optimizes latency-sensitive operations locally while leveraging cloud resources for complex analytics and model training. The hybrid model addresses many limitations of purely edge-based or cloud-based systems, though it introduces architectural complexity and integration challenges.
From a cost perspective, built-in systems require higher upfront hardware investments but lower operational costs. Cloud systems offer lower initial costs but higher recurring expenses. Hybrid systems present moderate upfront costs with optimized operational efficiency. Regulatory considerations vary significantly across architectures, with built-in systems generally facing fewer compliance hurdles compared to cloud-based solutions that must address data transmission and storage regulations.

Introduction
The convergence of artificial intelligence and medical technology represents one of the most significant advances in modern healthcare. As medical devices become increasingly sophisticated, the question of where and how AI processing occurs has become critical to system design, performance, and regulatory compliance. The choice between built-in device AI, cloud-based processing, and hybrid architectures fundamentally impacts patient care delivery, data security, operational costs, and clinical workflow integration.
Medical device manufacturers and healthcare institutions must navigate complex decisions regarding AI implementation strategies. These decisions directly affect diagnostic accuracy, treatment speed, data privacy, and overall healthcare outcomes. The FDA has approved over 950 AI-enabled medical devices as of 2024, representing a 400% increase from 2019, highlighting the rapid adoption and evolution of these technologies.
Built-in AI systems process data locally within the medical device, eliminating network dependencies and reducing latency to microseconds. This approach aligns with traditional medical device paradigms where reliability and immediate response are paramount. Companies like GE Healthcare have integrated AI directly into imaging systems, enabling real-time image enhancement and automated measurements without external connectivity requirements.
Cloud-based AI systems leverage distributed computing resources to perform complex analytical tasks beyond the capabilities of individual devices. These systems excel in applications requiring massive computational power, such as genomic analysis, population health analytics, and machine learning model training. The cloud approach enables continuous algorithm updates and facilitates collaborative research across multiple institutions.
Hybrid architectures represent an evolutionary approach that strategically distributes AI workloads between edge devices and cloud infrastructure. This model optimizes performance by executing time-critical operations locally while offloading computationally intensive tasks to cloud resources. The hybrid approach addresses limitations inherent in purely edge-based or cloud-based systems, offering a balanced solution for complex medical applications.
Regulatory frameworks continue to evolve alongside technological advances. The FDA’s AI/ML guidance emphasizes the importance of algorithm transparency, validation methodologies, and post-market surveillance. HIPAA compliance requirements vary significantly based on data processing location and transmission methods, influencing architectural decisions for AI implementation in healthcare settings.
This analysis provides healthcare technology professionals, medical device engineers, and healthcare administrators with comprehensive insights into the advantages, disadvantages, and implementation considerations for each AI architecture approach. Understanding these trade-offs is essential for making informed decisions that optimize patient outcomes while maintaining regulatory compliance and operational efficiency.

Medical Device AI Built-in Systems
Architecture and Technical Implementation
Built-in medical device AI systems integrate artificial intelligence processing capabilities directly within the device hardware, creating self-contained diagnostic and analytical units. These systems typically employ specialized processors such as Graphics Processing Units (GPUs), Tensor Processing Units (TPUs), or dedicated AI accelerators like NVIDIA’s Jetson series or Intel’s Movidius chips. The architecture includes optimized neural network models that have been compressed and quantized for efficient edge execution while maintaining clinical accuracy.
The technical implementation involves embedding pre-trained machine learning models into the device firmware or software stack. These models are typically trained on large datasets in controlled environments before deployment, then compressed using techniques such as pruning, quantization, and knowledge distillation to reduce computational requirements. The resulting models can perform inference tasks locally without requiring external connectivity or data transmission.
Edge AI processing leverages specialized hardware architectures optimized for parallel computation and low power consumption. Modern AI accelerators can deliver up to 100 TOPS (Tera Operations Per Second) while consuming less than 30 watts of power, making them suitable for portable and battery-operated medical devices. The processing pipeline typically includes data preprocessing, feature extraction, model inference, and result interpretation, all executed within milliseconds.
Advantages with Detailed Explanations
Ultra-Low Latency Performance
Built-in AI systems achieve processing latencies as low as 1-10 milliseconds, compared to 50-200 milliseconds for cloud-based systems. This performance advantage is critical for real-time applications such as arrhythmia detection, where immediate response can be life-saving. The elimination of network transmission delays ensures consistent performance regardless of connectivity conditions.
Enhanced Data Privacy and Security
Patient data remains within the device throughout the analysis process, significantly reducing privacy risks associated with data transmission and cloud storage. This approach inherently complies with data localization requirements and minimizes exposure to cyber threats targeting network communications. The self-contained nature of processing eliminates the risk of data interception during transmission.
Network Independence
Built-in systems function reliably in environments with limited or unreliable network connectivity, including rural healthcare facilities, emergency response situations, and developing regions. This independence ensures consistent diagnostic capabilities regardless of infrastructure limitations, making advanced AI-powered diagnostics accessible in resource-constrained environments.
Predictable Operating Costs
Once deployed, built-in AI systems incur minimal ongoing operational expenses, as they do not require cloud computing resources or data transmission fees. The cost structure is primarily front-loaded in the initial device purchase, making long-term budgeting more predictable for healthcare institutions.

Disadvantages with Real-world Implications
Limited Computational Resources
Edge devices face inherent constraints in processing power, memory, and storage capacity compared to cloud infrastructure. Complex algorithms requiring extensive computational resources, such as 3D image reconstruction or multi-modal data analysis, may be impractical for edge deployment. This limitation restricts the sophistication of AI models that can be implemented locally.
Model Update Challenges
Updating AI models in built-in systems requires device recalls, firmware updates, or complex over-the-air update mechanisms. This process can be time-consuming, expensive, and may require regulatory approval for each update. In contrast to cloud systems where models can be updated instantaneously, edge devices may operate with outdated algorithms for extended periods.
Scalability Limitations
Each device requires individual hardware investment and maintenance, making large-scale deployment economically challenging. Healthcare systems seeking to implement AI across multiple departments or facilities face significant capital expenditure requirements and ongoing support costs for distributed edge devices.
Limited Learning Capability
Built-in systems typically operate with static models that cannot learn from new data without explicit updates. This limitation prevents continuous improvement based on local patient populations or emerging clinical patterns, potentially reducing diagnostic accuracy over time as medical knowledge evolves.
Real Examples and Case Studies
IDx-DR Diabetic Retinopathy Screening System
The IDx-DR system represents a landmark achievement in built-in medical AI, becoming the first FDA-approved autonomous AI diagnostic system in 2018. The system integrates AI processing directly into retinal imaging devices, analyzing fundus photographs to detect diabetic retinopathy without requiring specialist interpretation. Clinical trials demonstrated 87.4% sensitivity and 89.5% specificity, enabling primary care providers to perform specialist-level screenings.
Case Study: A rural clinic in Iowa implemented IDx-DR systems across five locations, reducing specialist referral wait times from 3-6 months to immediate results. The system processed over 2,000 screenings in the first year, identifying 312 cases requiring specialist care, with a false positive rate of only 10.5%.

GE Healthcare Edison AI Platform
GE Healthcare has integrated AI capabilities directly into multiple imaging modalities, including CT scanners, MRI systems, and ultrasound devices. The Edison platform provides real-time image optimization, automated measurements, and preliminary diagnostic assistance. The AI-powered Auto Positioning feature reduces scan setup time by 40% while improving image quality consistency.
Philips IntelliSite Pathology Solution
Philips’ digital pathology platform incorporates built-in AI for tissue analysis and cancer detection. The system processes whole slide images locally, providing pathologists with AI-assisted diagnosis suggestions within seconds. Clinical validation studies show improved diagnostic accuracy and reduced interpretation time by an average of 30%.
Cost Analysis – Built-in AI Systems
Initial Investment: $50,000-$500,000 per device
Annual Operating Costs: $2,000-$10,000 (maintenance, support)
Update Costs: $5,000-$25,000 per major algorithm update
5-Year Total Cost of Ownership: $70,000-$625,000 per device
Medical Cloud AI Systems
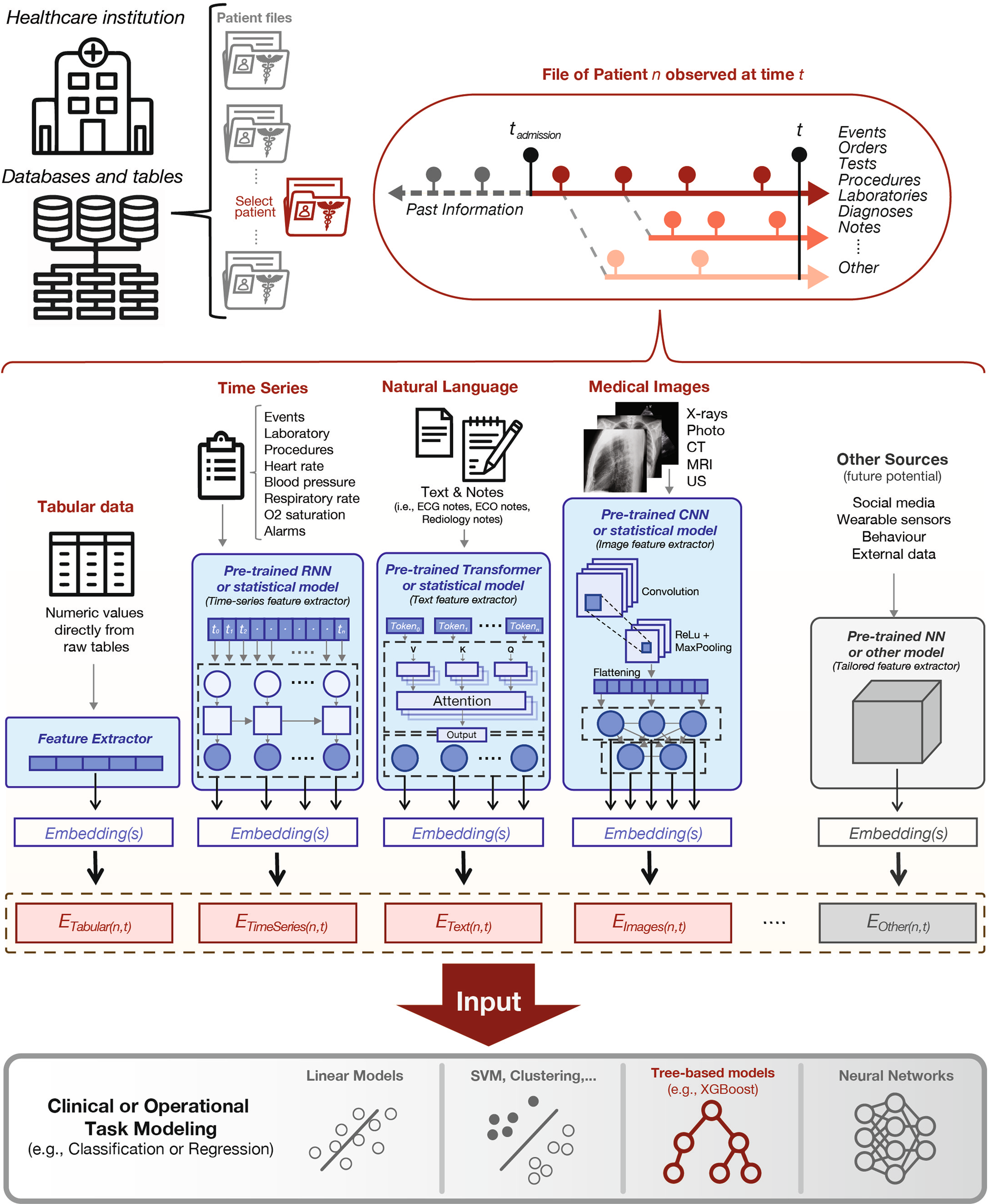
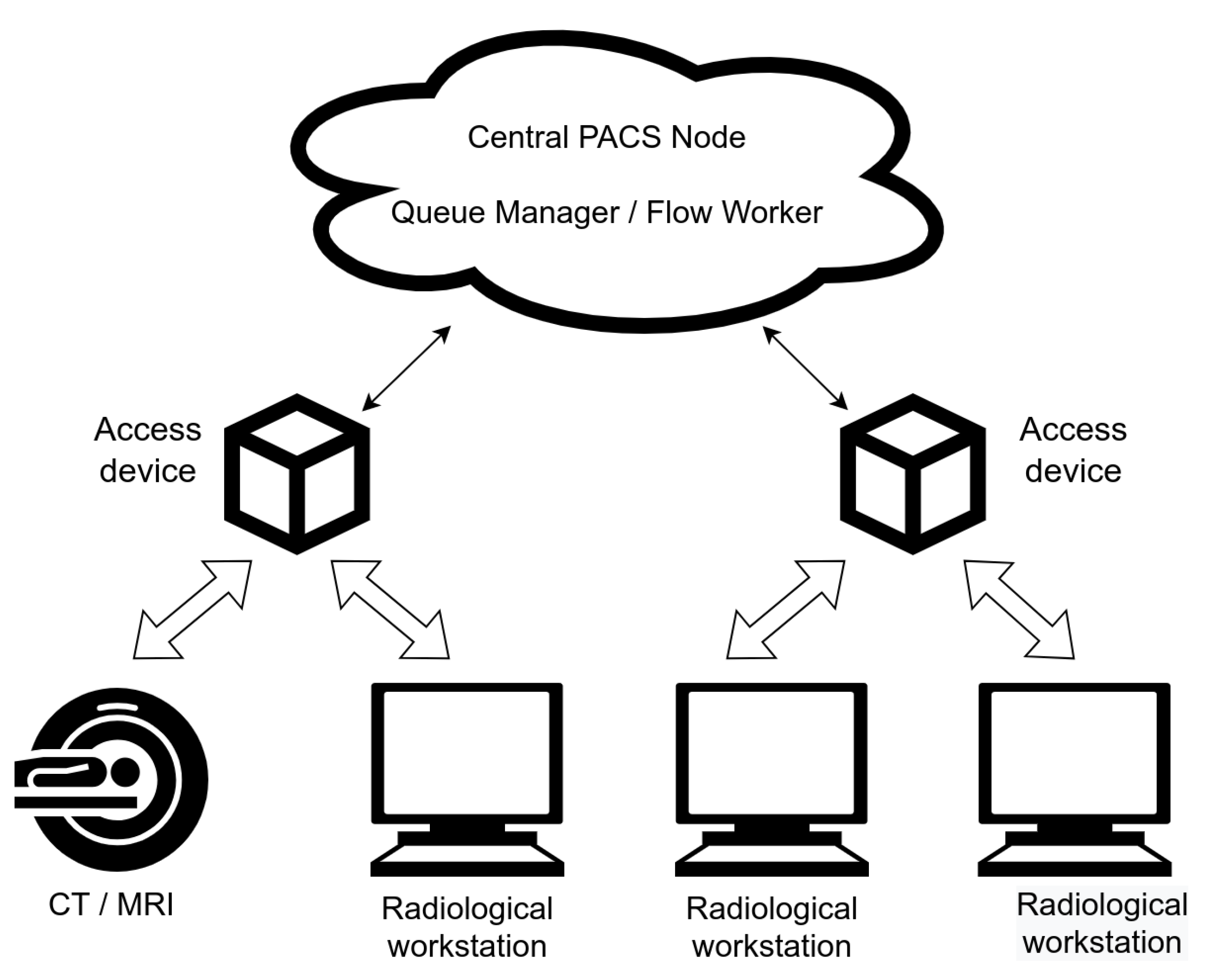
Architecture and Cloud Infrastructure
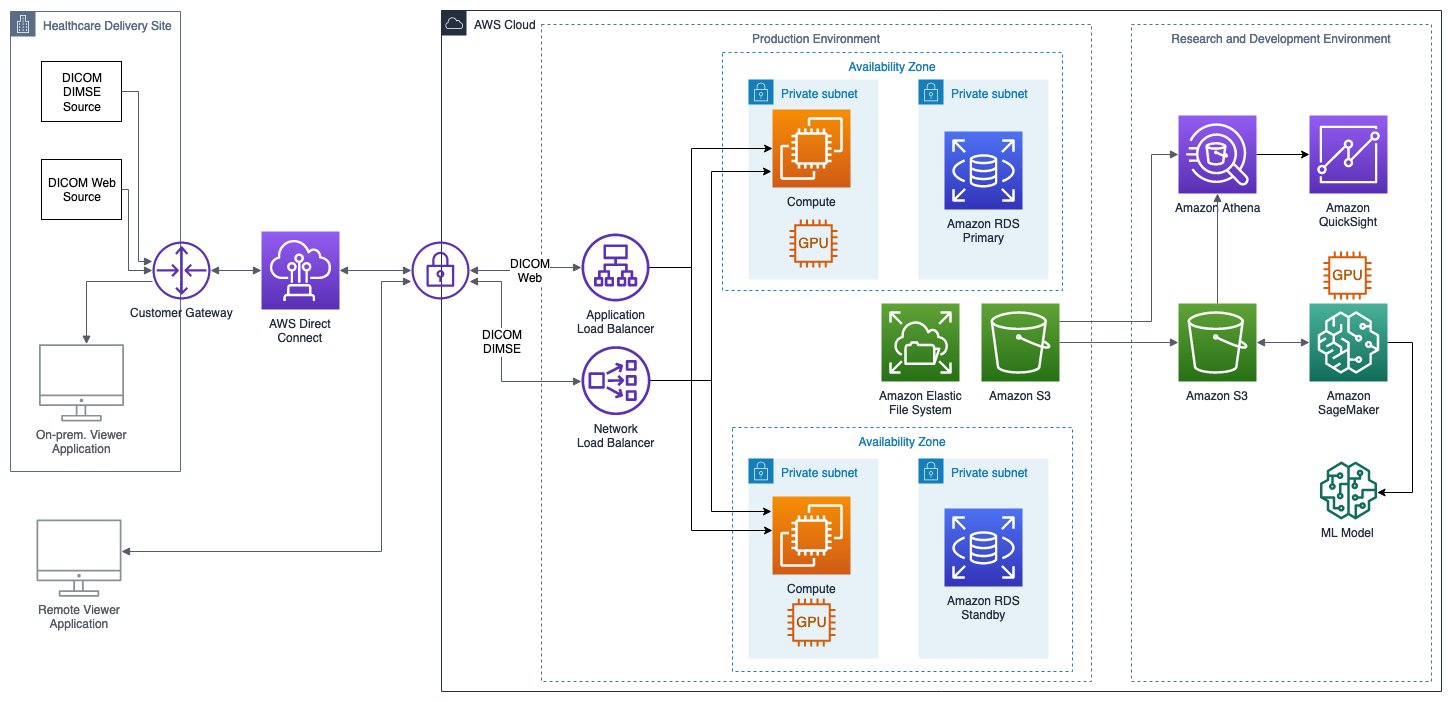
Medical cloud AI systems leverage distributed computing infrastructure to provide scalable, powerful artificial intelligence capabilities accessible through network connections. These systems typically employ multi-tier architectures including data ingestion layers, preprocessing services, machine learning inference engines, and result delivery mechanisms. Cloud providers such as Amazon Web Services (AWS), Microsoft Azure, and Google Cloud Platform offer specialized healthcare AI services with HIPAA-compliant infrastructure and advanced security measures.
The technical architecture incorporates auto-scaling compute clusters that can dynamically allocate resources based on demand. GPU-accelerated instances provide computational power exceeding 1,000 TOPS, enabling complex deep learning models that would be impossible to deploy on edge devices. Container orchestration systems like Kubernetes manage AI workloads across distributed infrastructure, ensuring high availability and fault tolerance.
Data processing pipelines handle DICOM images, electronic health records, genomic data, and other medical information formats through standardized APIs and secure transmission protocols. Advanced caching mechanisms and content delivery networks optimize performance for geographically distributed healthcare facilities, reducing perceived latency despite physical distance from processing centers.
Advantages Including Scalability and Collaboration
Unlimited Computational Resources
Cloud systems provide virtually unlimited processing power through elastic scaling capabilities. Healthcare institutions can access high-performance computing clusters with thousands of GPUs for complex analyses such as whole genome sequencing, radiomics analysis, or population health modeling. This computational capacity enables sophisticated AI models that exceed the capabilities of any single edge device.
Seamless Algorithm Updates
Cloud-based AI systems support instantaneous model updates across all connected devices and facilities. When improved algorithms become available or new clinical evidence emerges, updates can be deployed globally within hours rather than months. This capability ensures all users benefit from the latest advances in medical AI without device recalls or manual interventions.
Multi-institutional Collaboration
Cloud platforms facilitate secure data sharing and collaborative research across multiple healthcare institutions. Federated learning approaches enable model training on combined datasets while maintaining data privacy. This collaboration accelerates medical research and improves AI model accuracy through exposure to diverse patient populations and clinical scenarios.
Advanced Analytics and Insights
Cloud systems excel at population health analytics, epidemiological studies, and predictive modeling that require analysis of large datasets. These capabilities support public health initiatives, clinical research, and personalized medicine approaches that would be impossible with individual edge devices.
Cost-Effective Scaling
Pay-per-use pricing models allow healthcare institutions to scale AI capabilities based on actual utilization rather than peak capacity. Small clinics can access enterprise-grade AI capabilities without significant capital investment, democratizing access to advanced diagnostic tools.
Disadvantages Including Security and Latency Concerns
Network Dependency and Latency
Cloud systems require reliable high-speed internet connectivity, which may not be available in all healthcare settings. Network latency typically ranges from 50-200 milliseconds, making cloud solutions unsuitable for real-time applications requiring immediate responses. Network outages can completely disable AI capabilities, potentially impacting patient care.
Data Security and Privacy Risks
Transmitting patient data to cloud infrastructure introduces security vulnerabilities and privacy concerns. Despite encryption and security measures, data transmission creates potential attack vectors for cybercriminals. Regulatory compliance becomes more complex when patient data crosses geographical boundaries or involves third-party cloud providers.
Ongoing Operational Costs
Cloud services incur continuous costs for data storage, processing, and bandwidth consumption. High-volume healthcare institutions may face substantial monthly bills for cloud AI services, particularly for imaging-intensive specialties. Cost predictability can be challenging due to variable usage patterns and pricing structures.
Vendor Lock-in Risks
Healthcare institutions may become dependent on specific cloud providers’ proprietary technologies and APIs, making migration to alternative platforms difficult and expensive. This dependency can limit negotiating power and increase long-term costs as institutions become committed to particular vendor ecosystems.

Real Examples and Case Studies
Arterys Medical Imaging Cloud Platform
Arterys provides a comprehensive cloud-based AI platform for medical imaging analysis, offering FDA-cleared applications for cardiac MRI, liver analysis, and lung CT interpretation. The platform integrates directly with existing PACS systems and provides real-time processing of complex imaging studies. Clinical implementations have demonstrated 50% reduction in interpretation time for cardiac MRI studies while maintaining diagnostic accuracy.
Case Study: Stanford Medicine implemented Arterys for cardiac imaging analysis across multiple locations. The system processes over 500 studies monthly, reducing radiologist interpretation time from 45 minutes to 20 minutes per case. The cloud-based approach enabled sharing of expertise between campuses and provided 24/7 availability for emergency cases.
Google Medical Imaging Suite
Google Cloud’s Medical Imaging Suite provides AI-powered tools for medical image analysis, including automated organ segmentation, lesion detection, and quantitative measurements. The platform supports DICOM standards and integrates with major healthcare IT systems. Research collaborations with Mayo Clinic and other institutions have validated AI models for diabetic retinopathy, skin cancer detection, and breast cancer screening.
IBM Watson Health Imaging
IBM’s cloud-based imaging AI platform offers applications for medical image analysis across multiple specialties. The system provides population health insights and clinical decision support through analysis of large imaging datasets. Healthcare systems using Watson Health report improved workflow efficiency and enhanced diagnostic confidence through AI-assisted interpretation.
Cost Analysis – Cloud AI Systems
Initial Setup Costs: $10,000-$50,000 (integration, training)
Monthly Operating Costs: $2,000-$20,000 (processing, storage, bandwidth)
Per-Study Costs: $1-$10 depending on complexity
5-Year Total Cost of Ownership: $130,000-$1,250,000 (volume-dependent)
Medical Device Hybrid AI Systems
Hybrid Architecture Design
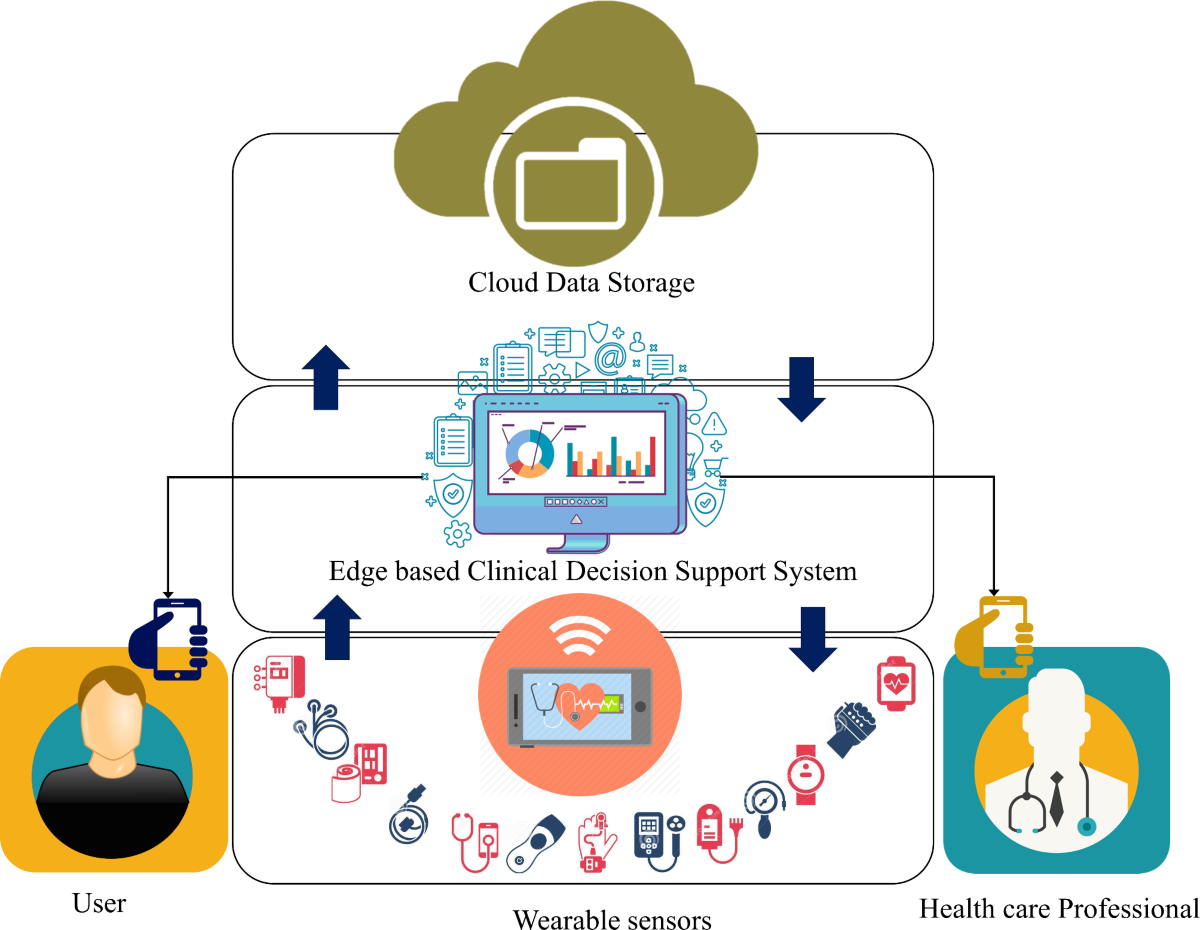
Hybrid medical AI systems strategically combine edge computing capabilities with cloud infrastructure to optimize performance, cost, and functionality. The architecture employs intelligent workload distribution algorithms that determine the optimal processing location based on factors including latency requirements, computational complexity, data sensitivity, and network availability. Edge components handle time-critical operations and preliminary analysis, while cloud resources manage computationally intensive tasks and long-term analytics.
The technical implementation utilizes edge orchestration platforms that can dynamically route AI workloads between local and remote processing resources. Modern hybrid systems employ containerized microservices architecture, enabling seamless migration of AI models between edge devices and cloud infrastructure based on real-time conditions. This approach maximizes the benefits of both deployment models while mitigating their individual limitations.
Data synchronization mechanisms ensure consistency between edge caches and cloud repositories while minimizing bandwidth consumption. Intelligent caching algorithms pre-position frequently accessed models and data on edge devices, reducing cloud dependencies for routine operations. When connectivity is available, systems can leverage cloud resources for model updates, complex analytics, and collaborative features.
Advantages Combining Edge and Cloud Benefits
Optimized Performance and Latency
Hybrid systems achieve optimal performance by executing latency-sensitive operations locally while leveraging cloud resources for complex analysis. Real-time monitoring and alarm functions operate at edge speeds (1-10ms latency) while comprehensive diagnostic analysis utilizes cloud capabilities. This approach ensures immediate response for critical situations while providing detailed insights when time permits.
Enhanced Reliability and Resilience
The dual-mode operation provides redundancy and fault tolerance. When network connectivity is compromised, systems continue operating using local processing capabilities. When edge resources are overwhelmed, cloud infrastructure provides additional capacity. This redundancy ensures consistent service availability regardless of infrastructure challenges.
Flexible Resource Allocation
Hybrid architectures enable dynamic resource allocation based on current needs and priorities. Emergency situations can trigger local processing mode for immediate response, while routine analysis can utilize cost-effective cloud resources. This flexibility optimizes both performance and operational costs based on clinical requirements.
Continuous Learning and Improvement
Edge devices can collect local data and usage patterns, which are periodically transmitted to cloud systems for model refinement. Updated models are then distributed back to edge devices, creating a continuous improvement cycle. This approach enables personalization for local patient populations while benefiting from broader clinical knowledge.
Balanced Cost Structure
Hybrid systems optimize costs by processing routine operations locally while utilizing cloud resources only when necessary. This approach reduces ongoing cloud expenses compared to purely cloud-based systems while avoiding the high upfront costs associated with fully-featured edge devices.
Disadvantages and Complexity Challenges
Architectural Complexity
Hybrid systems require sophisticated orchestration software to manage workload distribution, data synchronization, and failover procedures. This complexity increases development costs, testing requirements, and ongoing maintenance efforts. Healthcare IT departments must manage both local and cloud infrastructure components, requiring diverse technical expertise.
Integration Challenges
Implementing hybrid systems requires careful integration between edge devices, network infrastructure, and cloud services. Compatibility issues between different vendor technologies can complicate deployment and limit flexibility. Healthcare institutions may need to standardize on specific technology stacks to ensure seamless operation.
Security Complexity
Hybrid architectures present multiple attack surfaces requiring comprehensive security strategies. Data protection must be maintained across edge devices, transmission channels, and cloud infrastructure. Coordinating security updates and monitoring across distributed components increases the potential for vulnerabilities and requires specialized security expertise.
Regulatory Compliance Challenges
Hybrid systems must comply with regulations governing both local data processing and cloud-based operations. Regulatory approval processes may be more complex when systems operate in multiple modes with different data handling procedures. Documentation and validation requirements increase when systems can operate in various configurations.
Implementation Strategies
Tiered Processing Approach
Implement a tiered processing strategy where simple, time-critical operations execute locally while complex analysis occurs in the cloud. For example, vital sign monitoring and basic alarm functions operate on edge devices, while trend analysis and predictive modeling utilize cloud resources. This approach maximizes responsiveness for critical functions while leveraging cloud capabilities for advanced analytics.
Intelligent Data Management
Deploy smart data management systems that automatically determine which information requires local storage versus cloud processing. Sensitive patient data can remain on local devices while anonymized population data is transmitted to cloud systems for research and model training. This approach balances privacy requirements with analytical capabilities.
Gradual Migration Strategy
Begin with edge-heavy implementations and gradually increase cloud utilization as network infrastructure and security measures mature. This phased approach allows healthcare institutions to build expertise and confidence in hybrid systems while minimizing risks during initial deployment phases.
Cost Analysis – Hybrid AI Systems
Initial Investment: $30,000-$200,000 per deployment
Monthly Cloud Costs: $500-$5,000 (reduced utilization)
Edge Device Costs: $10,000-$50,000 per device
5-Year Total Cost of Ownership: $80,000-$500,000 per deployment
Comparative Analysis
| Criteria | Built-in AI | Cloud AI | Hybrid AI |
|---|---|---|---|
| Latency | 1-10ms (Excellent) | 50-200ms (Poor) | 1-50ms (Good) |
| Computational Power | Limited (10-100 TOPS) | Unlimited (1000+ TOPS) | Flexible (10-1000+ TOPS) |
| Network Dependency | None | Critical | Moderate |
| Data Privacy | Excellent | Moderate | Good |
| Update Flexibility | Poor | Excellent | Good |
| Initial Costs | High | Low | Moderate |
| Operating Costs | Low | High | Moderate |
| Scalability | Limited | Excellent | Good |
| Regulatory Complexity | Moderate | High | High |
Security Considerations
Security frameworks vary significantly across the three architectural approaches. Built-in systems benefit from air-gapped security but face challenges with security updates and vulnerability patches. Cloud systems leverage enterprise-grade security infrastructure but introduce transmission and storage vulnerabilities. Hybrid systems require comprehensive security strategies covering multiple attack surfaces while providing flexibility to adapt security measures based on data sensitivity and operational requirements.
Performance Metrics
Performance evaluation must consider multiple factors including processing speed, accuracy, reliability, and user experience. Built-in systems excel in consistency and immediate response but may lack the computational power for complex analyses. Cloud systems provide superior analytical capabilities but face variability due to network conditions. Hybrid systems offer balanced performance with the ability to optimize based on specific use cases and operational constraints.
Regulatory Summary
FDA Approval: Built-in systems typically require 510(k) clearance with fixed algorithms. Cloud systems face additional challenges for dynamic algorithms and require comprehensive validation of cloud infrastructure.
HIPAA Compliance: Built-in systems inherently comply through local processing. Cloud systems require Business Associate Agreements and comprehensive security measures. Hybrid systems need compliance strategies for both components.
Conclusion and Future Outlook
The choice between built-in, cloud-based, and hybrid AI architectures for medical devices depends on specific clinical requirements, operational constraints, and institutional priorities. Built-in systems excel in time-critical applications requiring immediate response and maximum data privacy. Cloud systems provide superior computational capabilities and collaboration features for complex analytical tasks. Hybrid architectures offer balanced solutions that optimize performance, cost, and functionality for diverse healthcare applications.
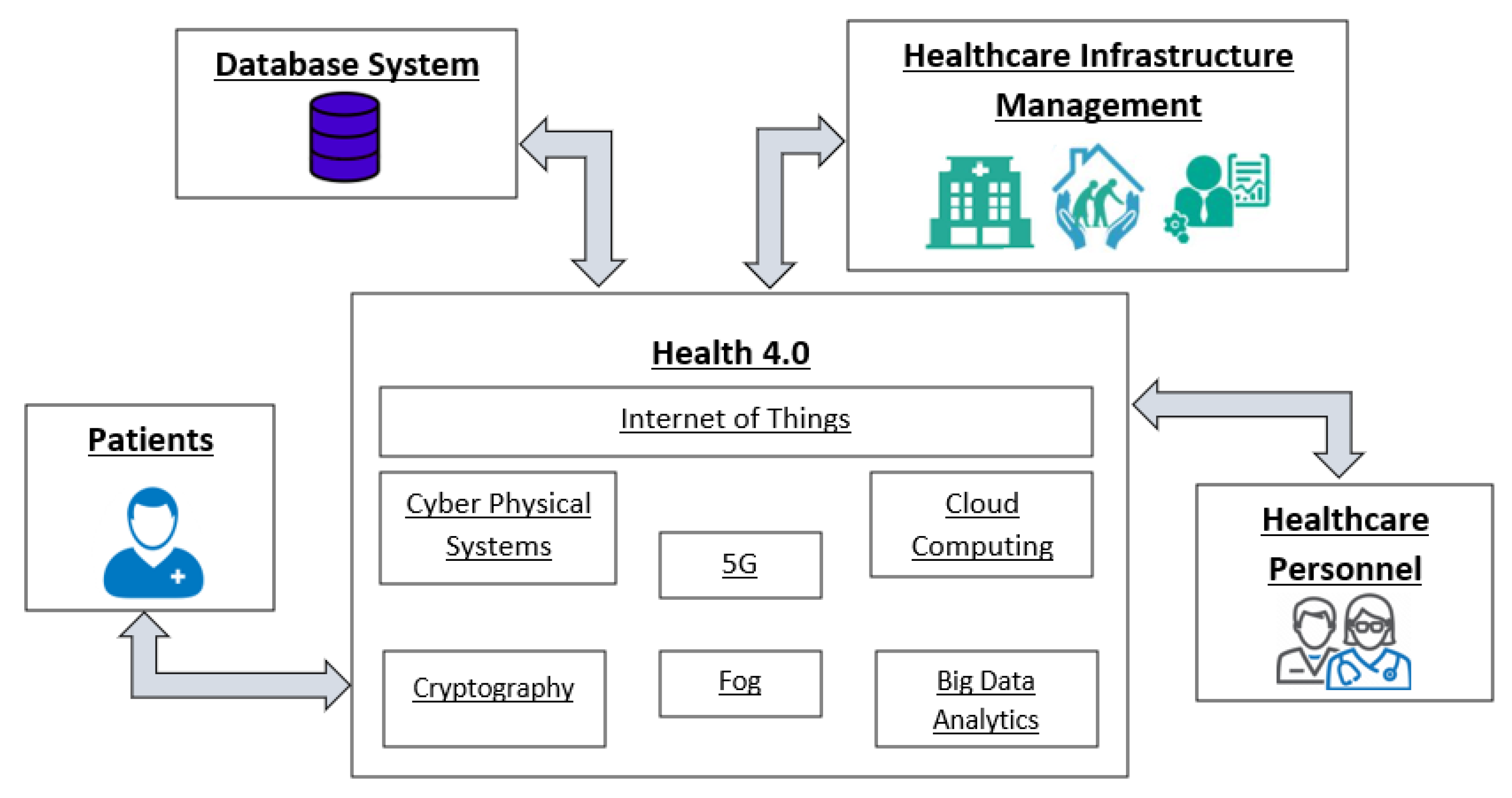
Future developments will likely focus on hybrid architectures that seamlessly integrate edge and cloud capabilities while addressing current limitations in complexity and integration challenges. Advances in edge computing hardware, 5G network infrastructure, and AI optimization techniques will continue to blur the boundaries between these architectural approaches, enabling more sophisticated and flexible medical AI implementations that better serve patient care objectives.